Executive Summary
The United States healthcare system is under immense pressure to meet the increasing demand for healthcare services with a shrinking, yet costly, workforce. Approximately ten thousand people turn 65 each day, and by 2030,1 all Baby Boomers—one of the largest U.S. generations, second to Millennials—will be at least 65. As the population ages, the number of people living with chronic disease is expected to increase. By 2050, the number of people living with at least one chronic disease is predicted to nearly double from 2020 figures, to nearly 143 million people. At the same time, the health workforce is anticipated to fall short of what is needed by up to 3.2 million health care workers by 2026. The combination of attrition due to burnout, retirement, and more flexible or lucrative careers, with an inadequate number of people in the health workforce pipeline threaten the United States’ ability to care for its population now and into the future. For the growing population of patients over 65 years old, who make up about 12 percent of the U.S. population but account for approximately 26 percent of all physician office visits, access to the appropriate level of care is of particular concern.
It’s not about the money, it’s about the time. We’ve had many providers leave for work-from-home telehealth roles for less money for the convenience of working from home. When our locations are open until 7:30, they want to leave at 7:30. But the charting and inventory slows them down and frustrates a lot of them.”
Meggen Brown MSN, FNP-BC, Chief Nursing Officer, Kroger Health
Artificial intelligence (AI) offers a powerful solution to the growing healthcare workforce shortage, helping to meet the demand for high-quality, cost-effective care. However, AI must be viewed as an enhancement—not a replacement—for human clinicians. The clinician-patient relationship is built on trust and empathy, elements that even the most advanced AI cannot replicate. Experts in healthcare and technology view AI’s value lying first in automating lower-value, delegable administrative and non-clinical tasks, freeing clinicians to focus on direct patient care and operate at the top of their license. Additionally, AI may one day extend beyond current applications in imaging to further support clinical decision making by providing real-time insights and synthesizing vast amounts of medical knowledge, supporting the delivery of evidence-based care.
“The [clinician]-patient relationship is sacred. It’s eroding in large part because [clinicians] just don’t have the time.”
Dr. Andy Wagner, Chief Medical Officer, Affineon
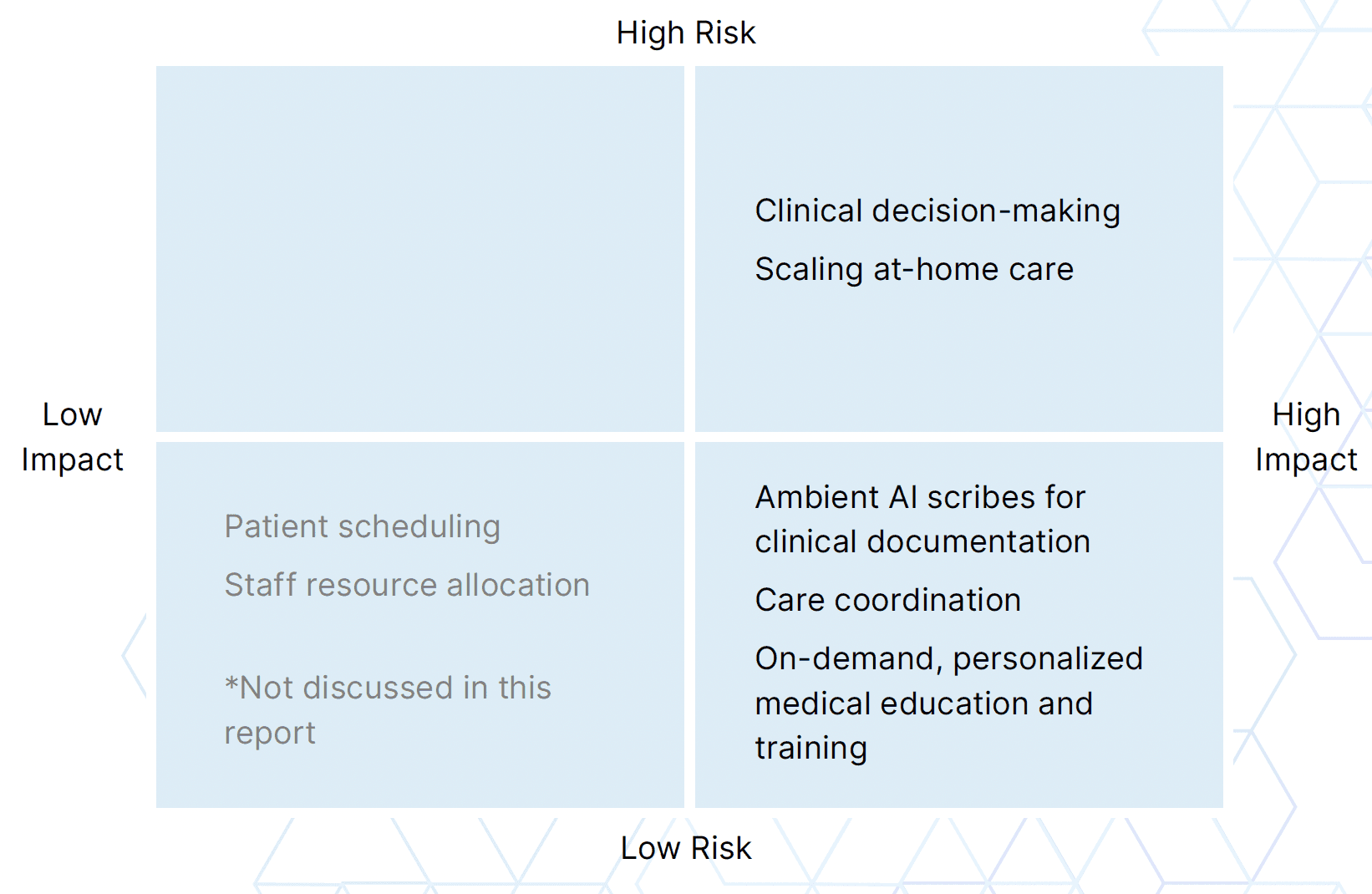
Possible use cases for AI in healthcare can be organized by two dimensions: risk, or the likelihood and severity of negative outcomes if the AI fails or is misused; and impact, or the scale of consequences, whether positive or negative. In this report, we identify five use cases across the risk gradient that have significant potential to transform how healthcare is delivered to extend and strengthen the health workforce and improve patient outcomes.
Low risk, high impact
Ambient AI scribes for clinical documentation
Care coordination
On demand, personalized medical education and training
High risk, high impact
Clinical decision-making
Scaling at-home care
Image 1: Risk and Impact Matrix of Possible AI Use Cases
Healthcare is a complex, highly regulated, and risk-averse industry. Realizing AI’s full potential at scale, for any use case, will require key conditions to be met by both the market and oversight authorities:
Reliable, transparent, and auditable AI models to ensure accuracy, build trust, and support accountability
Widespread adoption by healthcare organizations, clinicians, non-clinical staff, and—critically—patients
Uniform regulations that enable seamless interstate AI use, avoiding a fragmented, inconsistent landscape
Interoperable data and systems that allow AI to integrate seamlessly across electronic health records (EHRs), devices, and care settings
Modernized medical education and training that integrates AI into clinical practice and supports continuous, personalized learning
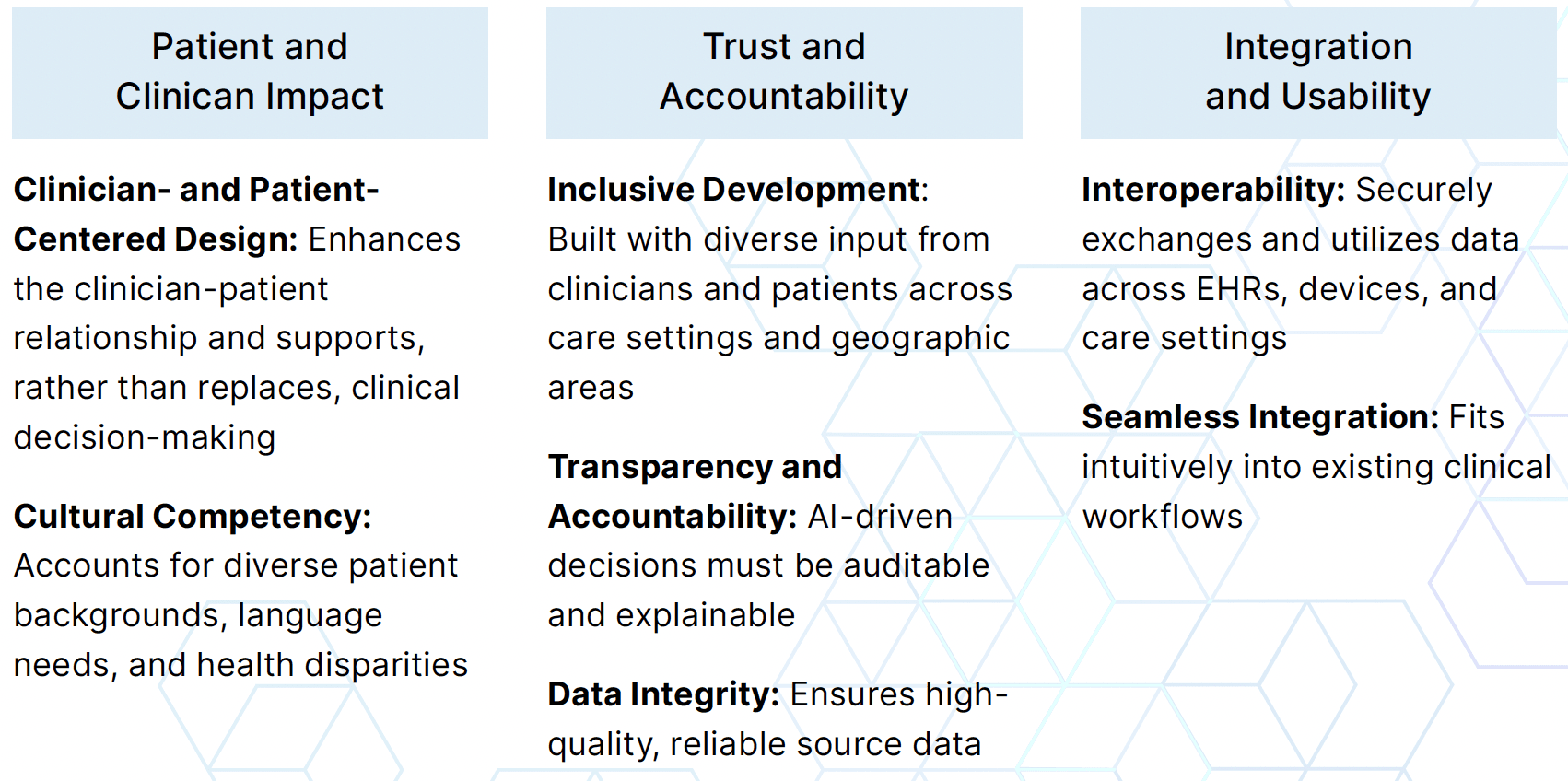
Finally, the immense potential of AI to enhance patient-centered care has led to a surge of solutions aimed at addressing healthcare’s most persistent challenges. To enable a more resilient and effective health workforce, AI tools must meet key criteria that fall into three categories: Patient and Clinician Impact, Trust and Accountability, and Integration and Usability.
Table 1: Key Criteria for Supporting a Resilient and Effective Healthcare Workforce with AI
Unlocking the Full Potential of the Healthcare Workforce with AI
To most effectively support the healthcare workforce, we must acknowledge an enduring truth of healthcare delivery: medicine is human. Thought leaders across the industry agree human providers will always have a place in healthcare because of the deep importance of trust and empathy in meaningful provider-patient relationships.
“It’s probably a bit counterintuitive to some that you’re going to use AI to bring humanity back to [healthcare] conversations…but it is intended to bolster that ability for the clinician to be more present and to make the decisions and to have the connections that need to be human in this environment.”
Matt Troup, Senior Director of Clinical Success, Abridge
With humans at the center of healthcare, the immediate opportunity for AI to support the healthcare workforce lies in ensuring healthcare professionals have the ability to focus on the patient. Impactful AI in the healthcare workforce assumes responsibility for tasks outside of the delivery of care to redirect the workforce’s time and energy back to the patient. Such AI use cases include ambient scribing for documentation, care coordination, medical education and training–with future potential for AI to assist in clinical decisions and scaling dispersed care.
Table 1: Key Criteria for Supporting a Resilient and Effective Healthcare Workforce with AI
Use Case 1: Ambient AI Scribes For Clinical Documentation
Since the widespread adoption of electronic health record (EHR) software, computers have become ubiquitous in exam rooms. While clinicians and patients appreciate the efficiency and accessibility of patient data, the EHR is also frequently cited as the leading contributor to burnout among clinicians. One study reports that nearly 75% of physicians with symptoms of burnout8 identify the EHR as the cause. Additionally, the emphasis on documentation during the patient encounter can negatively affect the quality of the clinician-patient relationship; use of the computer during an exam reduces eye contact, rapport, and limits clinicians’ ability to provide emotional support. Ultimately, disproportionate time clinicians spend on documentation vs. caring for patients disconnects them from the reasons they became healthcare workers.
Technology companies have taken notice of the need for a solution to the documentation burden that weighs down the healthcare workforce, leads to burnout, and ultimately drives current workers to leave and keeps others from pursuing a healthcare career. A leading example of the positive potential of AI is using ambient AI scribes for clinical documentation.
Description
Ambient AI is activated by a clinician at the start of a patient encounter, often using a smartphone. Once the AI is listening, the clinician is free to devote their full attention to the patient. After the visit, the clinician reviews the note that is autonomously generated by the AI for accuracy and actions that may be required, like making referrals and ordering prescriptions. The clinician is able to edit the note for clarity and factualness. The clinician is also able to give feedback to the AI to improve its performance, or to tailor the note’s format to the clinician’s preferences, like including bulleted lists.
Key Benefits
Reduces documentation time: One study estimates clinicians spend one hour on paperwork for every two hours of direct care. After rollout of an ambient AI scribe study, the New England Journal of Medicine reports11 that AI scribes do help reduce the time it takes for clinicians to construct notes each day.
May reduce burnout and increase healthcare worker retention: Athenahealth reports12 that two thirds of physicians feel overwhelmed because of the workforce shortage’s effect on administrative burden. Burnout is correlated with intent to leave the healthcare field; reducing burnout by addressing administrative burden could positively affect worker retention.
Restores connection between clinician and patient: Eliminating the need to document during the patient encounter strengthens the bond between patient and clinician. While it may seem counterintuitive, the use of AI scribes may result in a more human clinical experience.
Key Considerations
Auditability and transparency: Clinicians must have the ability to find the raw source for notes taken by ambient AI scribes for traceability purposes. This may be provided in the form of a transcript for a patient visit generated alongside the notes for the encounter.
Workflow integration: Notes from ambient AI scribes should have the ability to seamlessly transfer to EHR systems. The scribe’s interface must be as user-friendly as possible to minimize necessary training on the tool; the clinician should be able to download-and-go.
Use Case 2: Care Coordination
Because EHR software has become a significant part of clinicians’ training and delivery of care, patients now have a direct line to their care team—24 hours a day, 7 days a week. The EHR has contributed to a shortened timeline by which patients expect to receive communications from clinicians, including test results, referrals, scheduling questions, and other updates. In the absence of dedicated care coordinator roles, this kind of care coordination is often the primary responsibility of nurses, nurse practitioners (NPs), and physician associates (PAs) who are experiencing an increasing cognitive burden associated with these activities. One study finds that nurses spent the most time in the EHR outside of the patient’s room, indicating that care coordination for patients who are not physically in the practice at that time only adds to the current documentation burden. Another study directly shows that EHR usage increases nurses’ cognitive workload and translates to stronger feelings of exhaustion and burnout, which are only exacerbated by the additional EHR interactions required for patient care coordination activities.
The cognitive burden also affects patients and their level of satisfaction for the care they receive. An American Academy of Physician Associates (AAPA) study found that patients, especially younger adults, find managing their healthcare “overwhelming” and “time-consuming.” The overwhelm associated with care coordination can also prevent patients from getting the care they need; the same study found that more than two in five adults have skipped or delayed necessary care in the last two years and that patients who cannot schedule an appointment within the week often end up waiting one month for necessary medical appointments. Such barriers keep the healthcare workforce from providing adequate preventative care. When patients’ challenges with care coordination prevent necessary care from being addressed early on, clinicians are further burdened with urgent or emergency care when the patient’s condition worsens.
AI and automated care coordination solutions have become a promising opportunity to relieve the cognitive burden of manual care coordination for both clinicians and patients. Such tools can help get patients the answers they need in a more timely manner, while allowing clinicians to focus more of their time and attention on direct patient care.
Description
AI workflows can be embedded in EHR systems to automate communication for common care coordination tasks like sending test results, scheduling appointments and follow-ups, and communicating with other members of the care team. This support can extend beyond integration of an AI chatbot for patient-facing communications. For example, AI can automate the process of sharing a patient’s test results with other members of the care team. When a patient receives new test results or a new diagnosis, other clinicians they may be seeing are automatically alerted via the EHR system rather than by fax. This saves the patient time by avoiding the need to notify each member of their care team individually, and saves the clinician time when the automated workflow communicates with and provides updates to other members of the care team.
Key Benefits
Lift communication barriers between providers: The Journal of Patient Safety finds that miscommunication is a leading cause of medical errors. When AI supports care coordination, all members of a patient’s care team can be aligned on that patient’s history and needs.
Improve relationship between provider and patient: Both patients and providers experience cognitive burdens related to care coordination. Where 38% of healthcare organizations say they are not or only slightly effective in communicating with patients, AI-enabled care coordination can make healthcare answers feel more accessible to patients without added burden on clinicians.
Key Consideration:
Ability to triage: When integrating AI-enabled care coordination, especially in communication with patients, it is critical that these AI tools recognize questions they can and cannot answer. For example, responding to requests for scheduling and test results can be managed by AI care coordination models or agents, while questions about treatment plans or care decisions should be forwarded to clinicians.
Use Case 3: On-Demand, Personalized Medical Education and Training
Growing shortages in the healthcare workforce will only amplify the importance of preparing the next generation of healthcare workers. While students in medical education programs continue to learn the necessary technical skills for their license, there is an added level of complexity in medical practice for which students are not always prepared.
“There’s a care hands-on perspective, and that calls upon skill but also judgement. The whole ability to handle complexity is one of the areas of capacity we have to build. The ability to have discernment, prioritization, problem-solving; how do we begin to educate and train for that?”
Jennie Chin Hansen, Board Director, SCAN Health Plan
There is a clear opportunity for medical education to include a greater focus on helping students strengthen their ability to adapt in unpredictable healthcare environments. This involves getting students comfortable with their ability to weigh potential actions and prioritize next steps in a way that extends beyond what they’ve learned in a formal educational environment. Furthermore, effective clinical education itself must exhibit the ability to adapt. Industry initiatives like NYU Langone’s Program for Medical Education Innovations and Research Projects are pushing for medical education structures that provide real-world learning applications and training to anticipate future changes. This is an area primed for support from AI technologies through scenario development and simulation of clinical interactions.
Continued education is also an important consideration when evaluating the potential for AI to impact the healthcare workforce. Simulating healthcare problem-solving environments with AI, virtual reality, and augmented reality can upskill the healthcare workforce to help them proactively adjust to evolution in healthcare delivery such as changing patient demographics, technology advancements, and new research. Such AI-enabled case studies may supplement, or someday replace, continuing education requirements in an approach that is more personalized to each clinician’s individual strengths. Insight Global reports that a critical aspect of upskilling the healthcare workforce is to implement personalized learning paths, where continued education feels relevant rather than adding to cognitive burden.
Upskilling through personalized learning paths can be tailored to those in the healthcare workforce outside of licensed providers. There is an opportunity for AI to support career growth for administrative staff and other roles that are not directly related to patient care, appealing to their desire to help others and offering them a route to patient care and provider roles. This kind of ‘re-skilling’ will require practical, real-world training to support these people in applying their new knowledge, and AI can help develop such training tools. Constructing a path from non-medical role to clinician might bolster the shrinking healthcare workforce from within, leveraging individuals who already have a level of interest—and experience—in the industry.
Description
In medical education settings, AI can be used to simulate cases that students will likely encounter in their careers. For example, an AI browser extension may generate a situation based on a specific specialty that poses multiple potential treatment options for simulated patients. Based on the action chosen by the student, the AI tool will adapt the simulation to allow the student to navigate the effects of each decision while providing personalized feedback for each action. In a continuing education setting, clinicians may use AI to stay up-to-date on new research and technologies. For example, a surgeon might leverage an AI-enabled virtual reality headset to practice new surgery methods or tools in their specialty to receive feedback and become deeply familiar with them before transitioning to real patients. For members of the healthcare workforce who are not practicing providers, AI may develop a set of competencies that construct a pathway from their current role to potential desired roles as a clinician. This approach would not be meant to replace formal education, but rather reduce costs and accelerate the time needed to receive a formal education.
Key Benefits
Preparing for complexity: A BMC Medical Education study finds that medical students are often tasked with complex cases early in their transition to being a medical professional, leaving them feeling overwhelmed and overworked. When AI tools can better prepare medical students for the level of discernment clinical roles require, they may be more resilient in the face of these complexities.
Continuing education that resonates: The Journal of General Internal Medicine describes standards of care as changing rapidly and highlights that in practice, these standards may conflict at a public health versus individual level. In this environment, continuing education opportunities personalized to both provider and patient will support the workforce’s ability to deliver quality care.
Supporting workforce growth: With growing shortages in the healthcare provider workforce, enacting pathways to lift those already working in healthcare into medical provider roles will help the workforce strengthen from within—where workers already have a vested interest in the industry.
Key Considerations:
Ease of integration: To avoid additional cognitive burden on members of the healthcare workforce, AI tools that support education and training should be integrated with existing workflows in a way that does not require extensive additional training.
AI management training: While the tool itself should not require extensive additional training, there is still a need to support the healthcare workforce in their ability to get the most out of their AI tools. This may look like training on how to write effective AI prompts, where clinicians are taught how to communicate with AI tools in a way that allows them to receive the most benefit.
Mitigating bias: If AI is to be used in simulating real-world healthcare scenarios, the tool must be trained on diverse data that will reflect the types of patients the workforce will see in practice.
Use Case 4: Clinical Decision-Making
Especially given the pace of rapid advancements in AI technologies, AI will likely support clinical decision-making in the future. The speed at which research and medical publications are released has made it impossible for the healthcare workforce to remain updated on all new findings in their specialty—especially given the current administrative burden across the industry. MedCentral reports that a simple search of the word “diabetes” in the PubMed database yields over 52,000 results for papers published only in the first 10 months of 2023. The sheer volume of literature in healthcare is staggering, but uncovers a unique opportunity for AI to process large amounts of such text data to support clinicians’ decision-making.
Patient data is another equally vast dataset that providers are expected to leverage in clinical decision-making. A study at UW Health found that primary care physicians’ time reviewing patient EHR data outside of scheduled hours has increased 20%. Providing effective, informed patient care requires deep familiarity with their medical history, but manual review of patient data contributes to after-hours work and burnout, or may simply not be accessible. Here, AI-assisted patient data aggregation might help lift the EHR burden while empowering the healthcare workforce to make clinical decisions according to patients’ charts. Healthcare leadership is also expecting AI to contribute to clinical decision-making; a Deloitte study finds that 62% of healthcare leaders see promise in generative AI for quicker decision-making.
Description
The future healthcare workforce might leverage an AI summary tool that has the ability to absorb the newest developments in a given specialty from public databases while also aggregating an individual patient’s data to assist in making the optimal treatment decision for that patient. This tool is integrated with the EHR system, and uses a combination of current literature and past patient charts to draft clinical decisions for the provider’s review. The tool’s suggestions must be clearly traceable to the source material used to draft the decision.
Key Benefits
Risk management: The American Hospital Association reports that AI’s ability to analyze patient data and provide guidance to clinicians has outperformed conventional methods like the Modified Early Warning Score (MEWS) that have historically been used to manage patient risk.
Whole-health view of patient: AI tools can review patient history and relevant research exponentially faster than human providers, providing a more holistic view of a patient’s health and care needs without the associated time burden for providers.
Key Considerations
Ease of integration: Because EHR systems have become the central hub for patient care, successful AI tools for patient data aggregation and clinical decision-making will be seamlessly integrated with the EHR. They should be thought of as a built-in EHR capability rather than an additional workflow to learn how to use.
Provider oversight: Use of AI for clinical decision-making will require best practices regarding oversight from human clinicians and clear guidelines for the responsibilities of both the provider and the AI tool in clinical decisions.
Quality of source data: Clinical decisions made by AI tools should take into consideration the patient populations and cultures within the practice where they are implemented. Source data for training such AI models should therefore reflect a wide range of patient types.
Use Case 5: Scaling Distributed Care
The house call is being reimagined for the 21st century. Distributed care models, including telemedicine, hospital-at-home acute care, post-acute care, and remote patient monitoring, have gained significant traction, accelerated by the COVID-19 pandemic’s push for care delivery outside of traditional facilities. Several studies demonstrate the efficacy of these approaches. Hospital-level acute care at home, for example, not only costs less than facility-based care but also reduces readmissions and boosts patient activity levels. As importantly, it’s what patients want: a study shows two-thirds of patients offered hospital-at-home care choose it, citing increased comfort and proximity to family. From postpartum hypertension to cancer care, telemedicine and remote monitoring have consistently improved patient outcomes and expanded access, particularly in rural communities.
Description:
AI could transform distributed care by not only enabling its delivery but also identifying suitable patients. By synthesizing vast patient data and surfacing insights, AI empowers clinicians to confidently expand distributed care models. As discussed in AI’s role in care coordination, this technology is key to scaling distributed care, optimizing healthcare workforce utilization, and diversifying roles—all while lowering costs.
In this model, human healthcare workers would oversee a centralized command center, using AI to filter critical data signals from incoming patient information. Healthcare organizations would staff and oversee this command center, which would be considered an extension of patients’ care team. Beyond supporting clinicians in patient management and care planning, AI could function as a logistics coordinator, efficiently dispatching nurses, physical therapists, imaging technicians, and other care providers to patients’ homes. Additionally, AI-powered video monitoring could document at-home encounters, ensuring care quality and compliance.
Key Benefits:
Improving Access to Distributed Care: By helping clinicians be more sensitive in selecting patients for at-home care, AI can help more patients access its benefits, resulting in better outcomes.
Diversifying Healthcare Careers: Managing remote patient monitoring and care creates opportunities for healthcare workers to step into roles that may be able to be performed remotely and outside the facility, which may aid in efforts to retain and attract a qualified workforce.
Lowering the Cost of Care: By expanding access to at-home care, the high overhead costs of hospitalization, high staffing costs, and other indirect costs of hospitalization are reduced, thus lowering the overall cost of care without sacrificing patient outcomes.
Key Considerations
Ease of Integration: It is crucial for all the data collected by devices and tools used in remote patient monitoring at at-home care to be seamlessly integrated. Hospitals at the forefront of hospital-at-home care have worked around siloed datasets in their successful pilots, but this challenge must be resolved to achieve the promise of AI as a care enabler in this space.
“Last Mile” Care Coordination: While at-home care can be more efficient and cost-effective, its success isn’t guaranteed, especially as its applications expand. Non-traditional players like Best Buy are entering the healthcare space, leveraging their expertise in at-home services, much like their Geek Squad model.
Consistent Care Standards: Patients’ homes may vary greatly, possibly affecting the ease with which at-home care can be carried out. Additionally, at-home care providers, especially those earlier in their careers, may find it difficult to maintain consistent care standards over time. Ongoing feedback, adequate oversight, and flexible manuals for overcoming site-specific obstacles will be important to at-home care’s long-term success.
Market and Regulatory Requirements to Maximize AI’s Impact
Delivering healthcare requires navigating a complex, highly regulated, and heterogeneous system with often contradictory incentives. While the industry is traditionally cautious in adopting new technologies, significant tailwinds and growing enthusiasm are accelerating AI adoption. To fully realize AI’s potential at scale, key conditions must be met by both the market and oversight authorities.
“The margin for error in healthcare is narrower, so you want to be as certain as possible that new technology will have a positive impact. At the same time, adoption often hinges on incentives. Take electronic health records (EHRs) as an example—the biggest drivers of adoption included government incentives that essentially paid providers to implement EHRs. Healthcare is a complex ecosystem where incentives are not always as well aligned as they could be, which can slow the adoption of innovation.”
Dr. Aabed Meer, Senior Scholar and Clinical Assistant Professor, Stanford University
Reliable, transparent, and auditable AI models to ensure accuracy, build trust, and support accountability
Without trust in the AI models to be accurate, healthcare adoption will rightfully stall. Even when thinking of administrative tasks like medical coding or billing, the consequences of having a prior authorization denied because the AI tool failed to satisfy the necessary requirements can delay care, ultimately putting patients at risk.
All autonomously generated notes, lab summaries, communications with patients, and more should be able to be easily traced back to clinical source material.
Organizations like the Coalition for Health AI (CHAI)32 are developing standards for healthcare AI tools. Healthcare organizations and government regulators may find it necessary to establish their own standards.
Widespread adoption by healthcare organizations, clinicians, non-clinical staff and—critically—patients
The promise of AI in healthcare depends on most healthcare organizations and providers to opt in. To maximize its impact, incentives must be aligned so that all stakeholders experience tangible benefits:
Healthcare organizations: Cost savings, operational efficiencies, and improved patient outcomes.
Clinicians: Reduced administrative burden, enhanced patient care, and better patient outcomes.
Patients: Higher-quality care, improved health outcomes, and a more personalized experience.
Non-clinical staff: Greater efficiency, time savings, and expanded career opportunities.
Once a roster of use cases have been established and adoption reaches a tipping point, government agencies like the Centers for Medicare Services may need to further incentivize healthcare organizations to adopt certain AI tools, similar to how it incentivized use of EHR software.
Uniform regulations that enable seamless interstate AI use, avoiding a fragmented, inconsistent landscape
The healthcare industry already operates under a patchwork of state laws that define clinicians’ scope of practice. These current inconsistencies create real access to care issues in most states. Additionally, as telemedicine becomes essential for patient care and healthcare organizations seek to scale distributed, at-home care with AI, inconsistent licensure laws could pose a significant barrier to progress.
Interoperable data and systems that allow AI to integrate seamlessly across electronic health records (EHRs), devices, and care settings
Healthcare interoperability is already a topic that is top of mind for many, as EHR adoption has increased to include nearly 4 in 5 office-based physicians and nearly all non-federal acute-care hospitals (96%), and patients expect seamless access to their healthcare data in one place, regardless of where they received care.
A Centers for Medicare and Medicaid Services (CMS) rule, going into full effect in 2027, requires healthcare organizations and payers that accept or insure Medicare or Medicaid recipients, to implement and maintain certain Health Level 7® (HL7®) Fast Healthcare Interoperability Resources® (FHIR®) application programming interfaces (APIs) to streamline the exchange of healthcare data. While this is a step in the right direction, it leaves the commercially insured market largely untouched. As we have discussed, every effort must be made to ensure standardization across the healthcare system.
Modernized medical education and training that integrates AI into clinical practice and supports continuous, personalized learning
While AI tools should be intuitive enough to use without training, formal education must also evolve to incorporate AI and support change management across the healthcare industry. Just as clinicians learn to care for patients and collaborate with colleagues, they must also develop proficiency in using AI—whether as a teammate or a tool. Ignoring AI’s potential to personalize education would mean missing a significant opportunity to deliver high-quality, tailored instruction that meets learners’ needs.
Key Criteria for Supporting a Resilient and Effective Healthcare Workforce with AI
Technology in healthcare is evolving rapidly, making it difficult to predict how AI applications will develop in the coming years. This report outlines potential use cases across varying levels of impact and risk, but the healthcare workforce will likely adopt AI in ways beyond what is covered here. In such a dynamic landscape, three key areas of inquiry can help assess and identify AI solutions that strengthen a resilient healthcare workforce.
Patient and Clinician Impact
Medicine is deeply human. AI tools used to support healthcare workforce should assume responsibility for aspects of care that prevent clinicians from connecting with their patients. Successful AI integration helps the healthcare workforce redirect a higher proportion of their time and energy to patient care that only they as humans can provide.
What to look for
Clinician- and Patient-Centered Design: Enhances the clinician-patient relationship and supports, rather than replaces, clinical decision-making
Cultural Competency: Accounts for diverse patient backgrounds, language needs, and health disparities
Trust and Accountability
Healthcare is a highly regulated industry. For an AI solution to effectively navigate this environment, its analyses must be auditable and traceable to protect the members of the healthcare workforce and patients it will serve. Trustworthy AI healthcare solutions will provide a roadmap for where its decisions came from and why.
As the adage goes, garbage in means garbage out. The data on which AI models are trained must reflect the types of patients and cases the healthcare workforce will see in the real world. Culturally-competent AI will be trained on source data that includes a wide range of patient circumstances, backgrounds, and treatments.
What to look for
Inclusive Development: Built with diverse input from clinicians and patients across care settings and geographic areas
Transparency and Accountability: AI-driven decisions must be auditable and explainable
Data Integrity: Ensures high-quality, reliable source data
Integration and Usability
Overwhelm and burnout are already significant barriers in the healthcare workforce, and contribute directly to the need for AI support. AI solutions should therefore integrate smoothly with current workflows, require minimal additional training, and incorporate an intuitive, user-friendly interface. Seamless integration of data and tools also makes it possible for the AI to maximize its ability to synthesize large amounts of data to augment human healthcare providers. Providers will have a desire to understand how these AI tools are using current infrastructure to feel confident in the outcomes they generate, and to build patients’ trust in the use of these tools.
What to look for
Interoperability: Securely exchanges and utilizes data across EHRs, devices, and care settings
Seamless Integration: Fits intuitively into existing clinical workflows
Transparency: How and to what extent the AI is integrated is clear
For more information on how to join the movement to transform the healthcare landscape and its workforce, go to healthforce.org.
References
U.S. Census Bureau. (2019, December 10). By 2030 All Baby Boomers Will Be Age 65 or Older. https://www.census.gov/library/stories/2019/12/by-2030-all-baby-boomers-will-be-age-65-or-older.html
Ansah, J. P., & Chiu, C.-T. (2023). Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC9881650/
American Hospital Association. (2021, May 26). Fact sheet: Strengthening the health care workforce. https://www.aha.org/fact-sheets/2021-05-26-fact-sheet-strengthening-health-care-workforce
Agency for Healthcare Research and Quality. (2023, March). Physician Burnout. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
National Academies Press (U.S.). (2008). Retooling for an Aging America: Building the Health Care Workforce. https://www.ncbi.nlm.nih.gov/books/NBK215400/
Campbell, E. G., Regan, S., Gruen, R. L., Ferris, T. G., Ehrenfeld, M., Rao, S. R., & Wulf, W. A. (2016). Professionalism in medicine: a national assessment. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC4732308/
Budd, J. (2023, April 19). The Benefits of Mentorship in the Workplace. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10134123/#bibr9-21501319231166921
Budd, J. (2023, April 19). Burnout Related to Electronic Health Record Use in Primary Care. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10134123/#bibr10-21501319231166921
Kazmi, Z. (2013). Effects of exam room EHR use on doctor-patient communication: a systematic literature review. https://pubmed.ncbi.nlm.nih.gov/24629654/
Sinsky, C., Colligan, L., Li, L., Prgomet, M., Reynolds, S., Goeders, L., Westbrook, J., Tutty, M., & Blike, G. (2016, September 6). Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. https://www.acpjournals.org/doi/10.7326/M16-0961?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
Tierney, A., Gayre, G., Hoberman, B., Mattern, B., Ballesca, M., Kipnis, P., Liu, V., & Lee, K. (2024, February 21). Ambient Artificial Intelligence Scribes to Alleviate the Burden of Clinical Documentation. NEJM Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.23.0404
Athenahealth. (2024, June 21). Healthcare staffing shortages a key concern for physicians. https://www.athenahealth.com/resources/blog/healthcare-staff-retention-challenges-burnout
Rada, M., Johnson, A., Small, D., & Mottola, G. (2019). The Impact of Electronic Health Record Use on Physician Efficiency and Time Utilization: A Systematic Review. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC6371290/
Rotenstein, L. S., Torre, M., Ramos, M. A., Rosales, R. C., Guille, C., Sen, S., & Mata, D. A. (2020). Prevalence of Burnout Among Physicians: A Systematic Review. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC7153131/
AAPA. (2023, May 17). U.S. adults spend eight hours monthly coordinating healthcare, find system overwhelming. https://www.aapa.org/news-central/2023/05/u-s-adults-spend-eight-hours-monthly-coordinating-healthcare-find-system-overwhelming/
AAPA. (2023, May 17). U.S. adults spend eight hours monthly coordinating healthcare, find system overwhelming. https://www.aapa.org/news-central/2023/05/u-s-adults-spend-eight-hours-monthly-coordinating-healthcare-find-system-overwhelming/
Starmer, A. J., Sectish, T. C., Simon, D. W., Keohane, C., McSweeney, M. E., Chung, E. Y., ... & Landrigan, C. P. (2022). Frequency and Nature of Communication and Handoff Deficiencies in Medical Errors: A Systematic Review. Journal of Patient Safety, 18(2), e447–e455. https://journals.lww.com/journalpatientsafety/abstract/2022/03000/frequency_and_nature_of_communication_and_handoff.9.aspx
PricewaterhouseCoopers. (n.d.). Care management of the future is personalized, digital, and consumer-centric. https://www.pwc.com/us/en/industries/health-industries/library/assets/pwc-care-management-of-the-future-is-personalized-digital-and-consumer-centric.pdf
NYU Grossman School of Medicine. (n.d.). Research Projects. Program for Medical Education Innovations and Research. https://med.nyu.edu/departments-institutes/medicine/divisions/general-internal-medicine-clinical-innovation/program-medical-education-innovations-research/research-projects
University of Central Florida College of Nursing. (n.d.). Simulation Labs & Classrooms. https://nursing.ucf.edu/about/simulation-labs-classrooms/
Insight Global. (2023, November 28). Upskilling, Reskilling, and Preskilling in Healthcare. Insight Global Blog. https://insightglobal.com/blog/upskilling-reskilling-and-preskilling-in-healthcare/
Insight Global. (2023, November 28). Upskilling, Reskilling, and Preskilling in Healthcare. Insight Global Blog. https://insightglobal.com/blog/upskilling-reskilling-and-preskilling-in-healthcare/
Rada, M., Johnson, A., Small, D., & Mottola, G. (2021). Electronic Health Record Use and Physician Burnout: A Systematic Review. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC8561904/
Bodenheimer, T., & Sinsky, C. (2014). From triple to quadruple aim: care of the patient requires care of the provider. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC4414682/
Tallent, A. (2023, November 13). The Growth of AI Tools in Clinical Decision-Making. MedCentral. https://www.medcentral.com/biz-policy/the-growth-of-ai-based-tools-in-clinical-decision-making
Bendix, J. (2024, January 23). You’re not imagining it: doctors are spending more time than ever in their EHRs. https://www.medicaleconomics.com/view/you-re-not-imagining-it-doctors-are-spending-more-time-than-ever-in-their-ehrs
Deloitte Center for Health Solutions. (2024, January 30). Overcoming generative AI implementation blind spots in health care. https://www2.deloitte.com/us/en/insights/industry/health-care/how-to-prepare-for-generative-ai-in-health-care.html
American Hospital Association. (2023, May 9). How AI Is Improving Diagnostics, Decision-Making and Care. https://www.aha.org/aha-center-health-innovation-market-scan/2023-05-09-how-ai-improving-diagnostics-decision-making-and-care
Levine, D. M., Ouchi, K., Maurer, K., Gleason, K., Newhouse, J. P., Ramelson, T. Z., ... & Patel, C. T. (2020). Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Annals of Internal Medicine, 172(2), 77–85. https://www.acpjournals.org/doi/10.7326/M19-0600
ASCO. (2023, April 6). Therapy for Stage IV Non-Small-Cell Lung Cancer Without Driver Alterations: ASCO Living Guideline, Version 2023.1. Journal of Clinical Oncology, 41(15), e51–e62. https://ascopubs.org/doi/10.1200/JCO.2023.41.16_suppl.1582
Best Buy. (2021, October 19). Best Buy to Acquire Current Health to Help Make Home the Center of Health. https://corporate.bestbuy.com/2021/best-buy-to-acquire-current-health-to-help-make-home-the-center-of-health/
Coalition for Health AI, Inc. (n.d.). Our Purpose. https://chai.org/our-purpose/

